Introduction:
Diffuse large B-cell lymphoma (DLBCL), is predominantly diagnosed in the elderly with a median age of diagnosis approaching the seventh decade of life. The prognosis for DLBCL has improved for all age groups, but less so for those over 75 years of age. The VHA (Veterans Health Administration) is one of the largest integrated provider of cancer care in the United States and its population, on average, is older than the general US population, giving us an unique advantage in exploring outcomes in elderly population.
Methods:
We reviewed 2036 medical records on patients that had a diagnosis code of some form of lymphoma between 2011 to 2017. Patients were randomly selected. Inclusion criteria was any veteran with atleast one entry in their records of selected ICD-9 and ICD-10 codes for lymphoma. Exclusion criteria included primary CNS lymphoma, other low grade variant lymphomas, diagnosis and treatment outside VHA, inability to determine if patient record met study criteria or inability to fill in critical fields of interest for the study. 971 patients were included. Data was manually abstracted by trained researchers. The Wilcoxon-Mann-Whitney test was used to compare median Overall Survival (OS) between two groups. All statistical comparisons were made using the R statistical analysis package. A level of significance of 0.05 was used for all the tests.
Results:
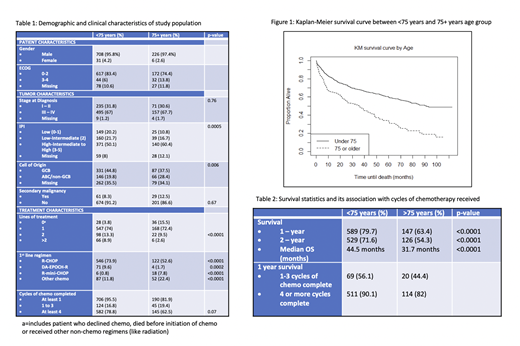
Of the 971 patients that met the inclusion criteria, 739 (76.1%) were <75 years and 232 (23.9%) were ≥75 years. Larger number of veterans were diagnosed at Stage III-IV (67% in <75 years and 67.7% in ≥75 years, p=0.76) with higher IPI score >3 (50.1 % in <75 years and 60.4% in ≥75 years, p=0.0005). Further descriptive comparison is outlined in Table 1.
Patients in the <75 years age group received more lines of chemotherapy (p<0.0001). The ≥75 years older age group was more likely to have no treatment or non-chemo treatment (15.5% vs 3.9%) and the under 75 group was more likely to have 2 or more lines of treatment (8.9% vs 2.6%).
For those who received chemotherapy, 82.4% in <75 years vs 76.3% in ≥75 years completed at least 4 cycles of therapy (p=0.07). However, 1 year, 2 years and median OS, was statistically different between the two age groups for all three measurements (p<0.0001) and survival decreases as age at diagnosis increases. (Table 2, Figure 1).
Conclusions:
Nearly 1/4th of the patient population were older than 75 years, and despite receiving comparable lines of chemotherapy, had lower survival when compared to patients who were <75 years. Previous studies (Lee et al, Cancer 2003 & Kenneth R.Carson et al, Blood 2012) have reported the role of an anthracycline or treatment related mortality contributing to inferior outcomes in the elderly population. While historical data supports CHOP at maximal doses in elderly, a re-assessment of dose intensity, role of anthracyclines and finding a balance between short-term efficacy and safety is a priority for this age group given increasing human longevity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal